No, the guidance clearly states the cancer review is a primary care review. The review is about the patient’s well-being, not about treating the cancer. It does not have to be a face to face review. It can be completed over the telephone. It should be about the patients individual health, support needs and the coordination between the sector.
Q&A
There could be two reasons for this.
- The cancer review has not taken place within 6 months of diagnosis.
- There has been a second diagnosis entered onto the patient’s record after the initial review. It could be either by the GP, Scanning clerk, data entry clerk or the note summariser.
It is important that all staff have an understanding of QOF to ensure duplicate entries are not recorded on a patient record.
You would need to check the patient’s records for the following:
- The patients review has taken place within the date criteria
- The patient has had a second entry for cancer. This could be due to a secondary cancer. You would need to change the episode to on-going so not to reactivate the review alert.
Over the counter medication should be re-coded annually to ensure that their situation has not changed. The Read codes are:
CTV3 Version 2
XaFsi 67I8. Advice about taking aspirin
XaF7N 8B3T. Over the counter aspirin therapy
XE0hr 8B63 Salicylate prophylaxis
Use the available exception for Aspirin, other alternative anti-platelets and anti-coagulant if not tolerated. The system will look at all three areas as if the patient cannot take one therapy, the system will look for the prescribing of the other groups of therapies that are listed within the criteria.
Why is a patient on CHD register with no diagnosis IHD made and normal angiogram in past, any ideas?
Without seeing the patient’s records, this is difficult to answer. This could be due an old entry, in the past GPs would put ‘Angina’ then free text ‘query angina’ . It will be a case of searching back in the patient’s clinical record to find the entry and mark it in error if appropriate.
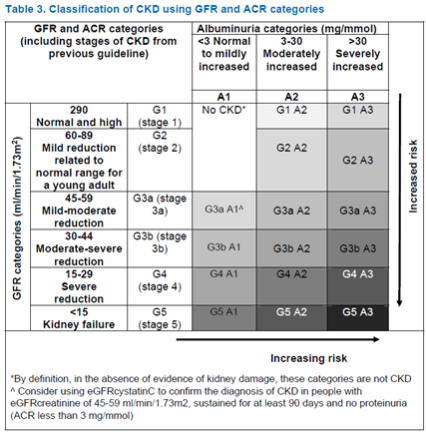
CKD diagnosis is to be based on a combination of two eGFR <60 and Albumin Creatinine Ratio (ACR) test results
NICE: Kidney function should be assessed using a combination of GFR and albumin: creatinine ratio (ACR) categories. Increased ACR and decreased GFR are associated with increased risk of adverse outcomes.
Eating a meal containing high protein can elevate creatinine. It is therefore recommended that patients do not eat meat in the 12 hours before their creatinine is measured and eGFR estimated.
https://www.nice.org.uk/guidance/cg182/resources/classification-table-msword-191901277
In the past we have always recommended to practices to use the CKD 2 Read code to remove a patient from the QOF register. The HSCIC have released a resolve Read Code in the V32 Business Rules, once added it will remove the patient from CKD disease Register.
| V2 | CTV3 | |
| Chronic kidney disease resolved | 2126E | XabuQ |
You should be using the following Read code. You need to add this code at the time of the MRC scale if =>3
V2: 44YA0 Oxygen saturation at periphery.
CTV3: X770D Oxygen saturation at periphery.
COPD does not resolve which is why there is not a code available, once you are diagnosed with COPD then you have it. Do not forget the patient may have both Asthma and COPD as 15% are expected to have both diagnoses.
If not it would be inappropriate labeling so the action would be to correct the diagnosis.
